Blog
Kirsty Chappell - UK Dental Professional & Athlete
Kirsty Chappell
Training for ‘Ironman’ in September 2022
2.4 miles swim
112 miles bike
26.2 miles run
Kirsty recently switched from mouth to nose breathing when she was training. Last week she completed a triathlon as part of her training and left this message.
Please click on play to listen.
Follow Kirsty on Instagram@kirstyssmileacademy


22nd June 2022
Please share this post on social media
Hay Fever!
Why this is the worst hay fever season on record?

By Tim Ives
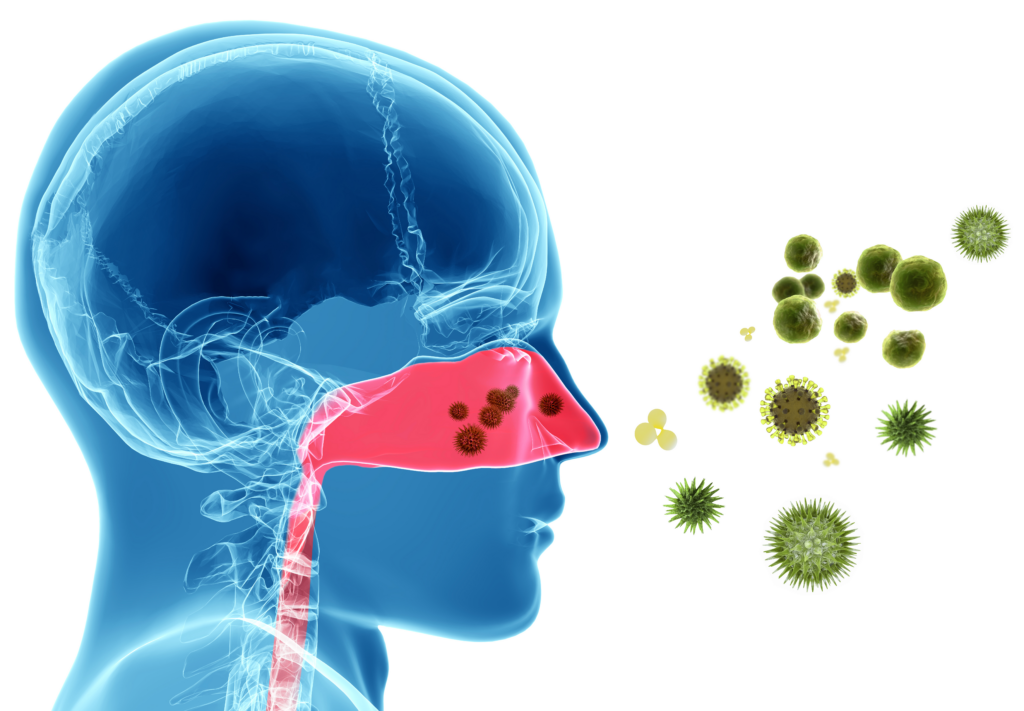
There has been a meteoric rise in hay fever related medication sales this year. Many people who have not previously suffered itchy eyes, sneezing, runny nose and sinusitis are now suffering. This is now affecting up to a third of the population!
During the pandemic people became indoor habitants and wore facemasks when venturing out of their homes. Whereas this may be good practice to prevent a virus infection, our immune systems became less busy and now when out and about we are over-reacting to harmless particles such as pollens and the result is higher levels of hay fever affecting many more people.
Hay fever in 2021 has been worse than ever for many people.
The medications of choice for many people are anti-histamine tablets and nasal sprays containing xylometazoline or oxymetazoline. Antihistamines cause everything to dry up which in the sinus cavity will open the door for harmful bacteria and potentially lead to a sinus infection. Many antihistamines also cause drowsiness and some blurred vision.

Nasal sprays containing xylometazoline or oxymetazoline cause the blood vessels inside the nose to contract and initially appear to relieve symptoms. They should not be used for more than a few days otherwise they create a rebound effect with the end result being a completely blocked nose. They also dry out the sinus area, like the tablets, leading to bacteria related infections.
Hay fever and head colds are the number one cause of switching someone from a nose to mouth breather, so maintaining clear nasal passages during hay fever season, 24 hours per day, can prevent more complex associated respiratory issues.
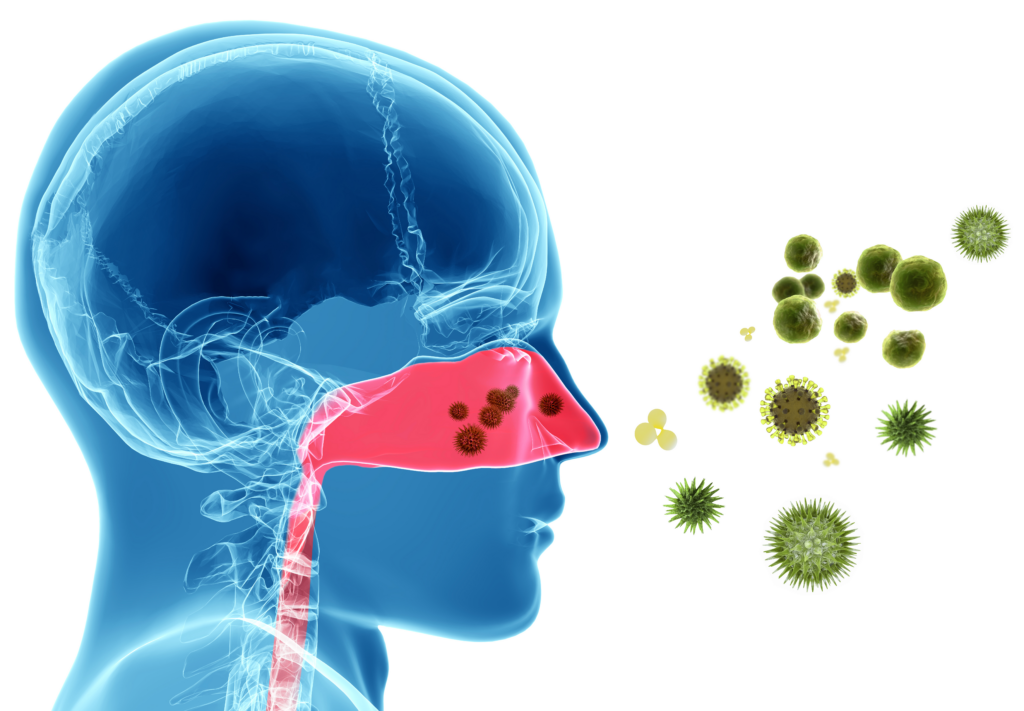
The key things to mitigate symptoms are:
Use Xlear nasal spray – this contains xylitol which will work with your body’s immune system by moisturising the nasal passages, washing out allergens and tackling harmful bacteria. This has no rebound effect and is safe for all ages from babies to seniors. Link to company website: Xlear
Myotape at night time – this is a specially designed tape that will ensure your mouth is closed whilst you sleep. See the previous blog below on Myotape.
Reduce the risk of inhaling pollen – wear a facemask whilst cutting the grass, gardening, driving etc. Close your windows. Wear sunglasses. Consider an air purifier.

25th June 2021
Please share this post on social media
The Oral Health Detective
Trisha was interviewed by Doug Jessop ABC4 Utah
Do you remember your dreams?

By Tim
What do dreams inform us about the quality of our sleep?
Firstly, dreams are very important and we all dream when we are asleep whether we remember them or not and we all dream between 3 to 6 times each night. It is believed that dreams play an important role in the memory function of the brain and also our cognitive process, so that is thinking, judging and problem solving.
We are also more likely to dream about events that happened during the day that are significant such as really sad or extremely happy occurrences but all dreams are a way for everyone to process the day’s events.

So what is a good sleep and how do we know if we have had one?
Ideally, adults should be asleep between 7-8 hours every night, children and especially teenagers need more. The sleep should consist of a 10-minute slow-wave sleep. This is the rapid eye movement (REM) part of sleep and usually occurs about 90 minutes after you fall asleep. During the REM cycle, the brain is extremely active and a couple of key things happen. Firstly almost 50% of human growth hormone (HGH) is released during the 10 minutes of slow-wave sleep. HGH is essential for normal growth and development in children and keeps adults looking young!
Your slow-wave sleep is also when you will have your most memorable dreams, so if you regularly remember your dreams, then this is a sure sign that you are having a healthy sleep.

It doesn’t necessarily mean that your sleep is poor if you don’t remember your dreams but it can be an indication especially if you are mouth breathing and/or snoring at night.

Mouth breathing and snoring are the two most common signs of sleep disordered breathing and both prevent you from entering your slow-wave sleep as you are much more likely to keep ‘semi-waking’. If you rarely get into slow-wave sleep, you’re missing out on that extremely important REM cycle. This may lead to extreme daytime sleepiness in adults and in children, irritability and anti-social behaviour. Also, adults are more likely to have bags under the eyes, and unwanted facial lines and wrinkles!
This post is dedicated to Faye Donald, RDH, who asked the question.

2nd June 2021
Please share this post on social media

By Tim Ives
Should metabolic syndrome include sleep-disordered breathing (SDB)?
According to research, the quick answer is yes.
Sleep-disordered breathing (SDB) is characterized by mouth breathing and/or snoring. This may progress to sleep apnea where there are pauses in breathing that vary in time depending on severity.
Metabolic syndrome is a term used to describe a combination of disorders that are typically associated with each other. These are currently:
Diabetes
High blood pressure
Increased waste circumference
Raised triglycerides – type of fat in blood that is unhealthy
Reduced denisty lipoprotein (HDL) – healthy protein that absorbs cholesterol
Raised plasma glucose

Research indicates that sleep disordered breathing (SDB) should be added to the metabolic syndrome list.

We considered for some time that people who are overweight have an increased risk of sleep disordered breathing because we believed the weight around the neck and collapsing soft tissues in the throat decreased the size of the airway and from the other perspective, people who are tired from poor quality sleep tend to snack more on carbohydrate rich foods in order to stay awake. So, in order to lose weight, quality of sleep should be taken into account and when looking to improve sleep quality, diet should be examined.

More recent research has indicated that SDB is far more complex than just being weight-related. Many people within a ‘normal’ weight threshold still get SDB, as is the case with cardiovascular disease, high blood pressure, and diabetes. SDB is associated with up to 200% increased odds of cardiovascular disease. There is a similar risk with diabetes for people with SDB and after treatment for SDB, there is typically a big improvement in diabetes and a reduction in blood plasma glucose.
Both children and adults suffering SDB show very low levels of oxygen in their blood (hypoxemia) which is now considered to be the central issue for a metabolic disturbance, demonstrating that SDB is contributing to metabolic dysfunction beyond the effects of just being overweight.
So, what does all of this mean? SDB can affect anyone and is not necessarily weight-dependent.
SDB should be included in the list of metabolic syndrome disorders and be considered as an important factor when considering a treatment plan for diabetes, high blood pressure, increased waste circumference and obesity.

10th May 2021
Please share this post on social media

By Tim Ives
Given that it looks like we will have another year before we will all have received the COVID-19 vaccine and we can return to the new normal, I would like to see a post-COVID world where we all become more mindful and speak more slowly. There are huge health benefits to this and it easy to achieve.
As a breathing practitioner, I have observed that the majority of people breathe incorrectly when speaking. I wonder if this is a 21st century problem as we feel under pressure to get to our point quickly?

As technology allows us to access information at light-speed I wonder if the ‘listener’ is becoming more impatient and the ‘speaker’ more pressurised to complete what they are saying as quickly as possible? When you next listen to radio shows or TV interviews, consider if you agree with me and also observe how the ‘speaker’ is breathing. I have also noticed that interviewers seem to try and hurry people along to make their point as quickly as possible. We seem to have less time for people to pause, accentuate and embellish their story and to paint a literary picture that we all find entertaining. For me, when listening to people, less is more and the more adjectives the better!
Nasal breathing when speaking is really essential to prevent a COVID-19 infection. Our nose provides us with an amazing filtration system that will trap and eliminate 98-99% of unwanted particles and micro-organisms such as bacteria and viruses, including the corona virus. If mouth breathing whilst speaking, any micro-organisms that are present, will be drawn directly into your lungs. In addition, when nose breathing, our sinus cavity releases a colourless gas called nitric oxide which is toxic to all micro-organisms. This is part of our natural defence mechanism which switches off if we start mouth-breathing. (See my previous blog on how we can increase nitric oxide production.) Our nose is a more effective filtration system than a face mask and we should all be nose breathing and wearing a face mask when appropriate. If you wear a face mask and mouth breathe, you are still increasing your risk of infection.

Really take the time to observe if you are breathing through your mouth or nose when taking a breath. If you discover that you are breathing through your mouth when speaking, the best way to switch to nasal breathing is to pause more regularly when speaking for a breath and speak slowly. Speaking slowly and clearly will also ensure people will fully understand you and you will discover that you are repeating yourself less often. Slowing down gives you more thinking time and nasal breathing will supply your brain with an additional 18% of oxygen. You may discover that, not only do you stay healthy but additionally your spoken word becomes more interesting to the listener as you become more expressive and descriptive.
Breathe slow and speak slow and give people time to express themselves. Why not make it your new year resolution?
Happy New Year.

5th January 2021
Please share this post on social media

By Tim Ives
In my previous blog which I posted in July, I mentioned the amazing ‘magic molecule’ nitric oxide (NO). This molecule is a colourless gas that was proclaimed ‘molecule of the year’ in 1992 and the 1998 Nobel Prize was awarded for discovering nitric oxide’s role as a cardiovascular signalling molecule.
This magic molecule, which kills viruses (including the Coronavirus) and bacteria is released in our sinus cavity when we breathe through our nose.1 NO also opens up the airways inside the nose and our lungs, which allows oxygen to travel effectively from the outside world to where it is needed inside our bodies. If we breathe through our mouth, NO production slows down and switches off, so we don’t get the amazing benefits that nose breathers get.
So, how do we increase NO production to keep us at maximum breathing health? The answer is to hum!

You can hum-along to anything but at this time of year, why not hum-along to your favourite Christmas tunes? The oscillating airflow caused by humming enhances sinus ventilation and increases NO levels by 15 times.2 That is an enormous increase!
Be sure to inhale in through your nose at the end of each hum.
Reminder of the key points to stay healthy and prevent respiratory problems:
a/ Make sure you breathe through your nose 24 hours per day, especially at night and whilst speaking.
b/ Clean you nose morning and night with a Xlear Nasal Spray.
c/ Start regular humming.

References:
- Martel J; Ko YF; Young J; Ojcius D. Could Nasal Nitric Oxide Help to Mitigate the Severity of COVID-19. Microbes Infect, Vol 22(4) 168-171, 2020
- Weitzberg E; Lundberg ON. Humming Greatly Increases Nasal Oxide. American Journal of Respiratory and Critical Care Medicine, Vol 166(2) 2002 accessed: https://doi.org/10.1164/rccm.200202-138BC
November 26th 2020
Please share this post on your social media
LipZip Book Review
We are really excited to have received this book review. Sarah is currently Senior Lecturer, Programme Lead in the Institute of Dentistry, Queen Mary University of London. Sarah was awarded an MBE for services to Oral Health in the New Year’s Honours List in 2017, which was presented by the Queen.

By Sarah Murray
Tim Ives, one of the co-authors, invited me to review his book, Lip Zip, which has provided me with considerable food for thought, following reading it a couple of times, and delving back into it at various points since.
The book is very appealing in that it is pocket sized, and is easily digestible and has an eye-catching cover.
It is split into sections that covers Tim and Trisha’s experiences in why they personally became interested in the topic of breathing, followed by a variety of real case studies, which are well considered, with the authors linking the theory behind each case, to enable a better understanding of this topic. The cases cover a broad spectrum of individuals, including children; we are all born with the ability to breathe correctly through our noses, and then often change to mouth breathing for a variety of reasons, with potentially significant side effects. Encouraging nose breathing using various strategies is discussed and the positive effects on the individuals is highlighted in each case.
I am sure there are aspects of the cases that resonates with each us individually, or people we know, much like Jacob, the technology engineer, who thought Trisha was referring to himself, during one of her lectures!
I particularly like the use of motivational interviewing that is used in a couple of the case studies, as this can be a powerful way to encourage behaviour change, and these reinforced this concept to me.
The final section focussed on the science and brings together the evidence to underpin the cases. This section requires more concentration as there is so much useful information to digest, to get the most out of the book. Aspects of sleep deprivation due to mouth breathing that links to ADHD, skeletal growth, and failure to thrive are all discussed. References are provided to encourage further reading.
I would recommend this book to all individuals interested in oral and general health and will assist all readers how to consciously breathe.
Sarah Murray MBE, SFHEA, MA, Dip DH, Dip DT
- October 23rd 2020
Please share this post on your social media

By Tim Ives and Trisha O'Hehir
According to Dr Stephen H. Sheldon, North-western University, USA and director of the largest children’s sleep clinic in the USA, “There is no such thing as ADHD, these kids are simply trying to stay awake.”
We all know how children behave when they are tired. When on holiday have you observed young children who were kept up far too late by their parents? They display the sort of behaviour that you may have described as ‘hyperactive’. Imagine how these children would behave if they never had a good nights’ sleep.
Key point. Children don’t know that they are having problems sleeping.
It is up to the parent/s to recognise that there is a problem. Have you ever moaned about your child forgetting to do simple tasks or chores? This is a classic example of Sleep Disordered Breathing (SDB). Have a listen if they are snoring or look to see if they have their mouth open when sleeping.



ADHD and SDB are completely different issues but both present similar signs and symptoms in children. Making a misdiagnosis in a child will have a big short-term negative impact and could have consequences that may affect them for the rest of their life.
The drug commonly prescribed for ADHD is Ritalin. Nearly 3 billion doses of this drug have been consumed. The side effects of Ritalin are:
Trouble sleeping
Nervousness
Loss of apatite
Vomiting
Headaches
What do you think would be the outcome if a drug that prevented sleeping was administered to a child with SDB?
So, what are the effects of SDB in children apart from being permanently tired, irritable and unable to concentrate? If children are not breathing correctly at night, for example, snoring or mouth breathing, they commonly fail to get into a deep sleep, termed slow wave sleep and spend the night having many small sleeps. Human growth hormone is released during slow wave sleep and this hormone is responsible for growth and development of the child. Reduction in human growth hormone due to SDB will prevent the child from developing as they should.
The specialist responsible for making an ADHD or SDB diagnosis should be the paediatrician, so could a paediatrician differentiate between SDB and ADHD? The answer to this question is mostly no. In a study of the members of the American Academy of Paediatrics which looked at sleep screening practices amongst paediatricians, researchers discovered that fewer than one in five had received any training in sleep disorders (1).
The sooner that an SDB diagnosis is made, the better. This can only be done by having a sleep study. This is the only way to differentiate between SDB and ADHD.
Doctor Karen Bonuck researched 11,000 snoring kids and studied them at 6, 18, 30, 42, 54 and 69 months. Children who had peak SDB symptoms before 18 months that resolved still predicted 50% increased odds of behaviour problems at 7 years (2). Snoring in babies is not cute and should be addressed immediately.
If you would like to discover more about breathing and how breathing related issues can affect babies, children and adults, we have a great on-line course that is available here: LipZip
- Faruqui, F., et al. Sleep disorders in children: a national assessment of primary care paediatrician practices and perceptions. Paediatrics. 2011. https://pediatrics.aappublications.org/content/128/3/539
- Bonuck, K., et al. Sleep-disordered breathing in a population-based cohort: behavioural outcomes at 4 and 7 years. Paediatrics 2012; 129: 1-9.
- October 13, 2020
Please share this post on your social media

Tim
For those of you who have read our book or taken our online course you will be aware that we have mentioned micropore tape and lip gel to help with various breathing related issues. For those of you who haven’t read our book or taken our online course here is a link: LipZip
Please click the video to see how easy it is to apply Myotape to the mouth.
- Prevents snoring
- Improves sleep apnea
- Suitable to use with CPAP
- Improves sleep quality and will reduce fatigue
- Helps prevent dental disease
Myotape is hypoallergenic and especially made for the skin.
Trisha and I would not advise this product to anyone under the age of 4 or anyone not able to remove the product by themselves.
Do not use any micropore tape, Myotape or sticky lip gel if you have:
- Tummy upset
- Consumed alcohol or sedatives
- Severe nasal congestion
- Severe heart condition
- Severe breathing problems
- 1st September 2020
Share this Post

Tim
Given the current COVID-19 global focus on face masks in order to prevent the spread of infection, I believe what is more important is the way we breathe when we are wearing and not wearing a mask. Nose breathing is our first line of defense against inhalation of micro-organisms as the majority will get trapped in mucous whereas anything directly inhaled into the lungs has the potential to stay there for up to 120 days. Mouth breathers also typically inhale 10 to 15 liters of air per minute compared to 4 to 6 litres for a nose breather (1). This huge difference in volume will definitely increase risk of COVID-19 infection for mouth breathers. It is also very easy to switch from nose to mouth breathing when wearing a mask, especially when in conversation. Keep those sentences short and ensure that you are breathing in and out through your nose when speaking.
Nitric oxide in the paranasal sinuses is taken into the lungs when nose breathing. (2) Mouth breathing bypasses this important molecule which is toxic to the Corona Virus. (3) Nose breathing is a key defense against infection.
Just to complicate matters the latest research from the University of North Carolina informs us that the receptor cells that COVID-19 requires to attach itself to the host are most abundant in the cells inside the nose and less abundant in the lungs. (4)
Obviously, mouth breathing and inhaling large volumes of air directly into the lungs to avoid COVID-19 attachment onto nasal cells is not a good way to mitigate infection. So, what is the best way to prevent COVID-19 attaching itself to the cells inside our nose?



Xlear, a USA based xylitol company, has been undertaking research at the Universities of Geneva and Utah State University to see if the containing xylitol, saline and grapefruit seed extract destroy the virus sprays are toxic to COVID-19. I have viewed the university reports (not published) and the sprays containing xylitol, saline and grapefruit seed extract destroy the virus and surprisingly it was the grapefruit seed extract that is the ‘active ingredient’ against COVID-19. Human trials are underway. Be sure to sign up for our newsletter as we will keep you in touch with these latest results.
In conclusion I believe we should all pay attention to the way we breathe and ensure we breathe through our nose (especially when speaking) and be cleaning our nasal cavity morning and night with Xlear Nasal Spray to prevent COVID-19 infection.
If you would like to learn more about breathing and its oral and general health effects, the computer screen icon at the top of this blog will take you to details for the consumer version of our online course.
(US English)
References:
1. McKeown P. The Oxygen Advantage. Harper Collins, NY, USA; 2015
2. Tornberg C; Marteus H; Schedin U; Alving K, Lundberg J; Weitzberg E. Nasal and Oral Contribution to Inhaled and Exhaled Nitric Oxide: A Study in Tracheotomized Patients. Eur Respir J, 19(5): 859–864, 2002.
3. Martel J; Ko YF; Young J; Ojcius D. Could Nasal Nitric Oxide Help to Mitigate the Severity of COVID-19. Microbes Infect, Vol 22(4) 168-171, 2020
4. Hou Y; Okuda K; et al. SARS-CoV-2 Reverse Genetics Reveals a Variable Infection Gradient in the Respiratory Tract. Cell Journal, Vol 182(2) 429-446, 2020. https://doi.org/10.1016/j.cell.2020.05.042
- 29th July 2020
Share this post

Nasal Breathing and Covid-19
Protect yourself from the Coronavirus by breathing through your nose. The nose is an amazing filter to keep viruses, bacteria, spores, pollen, and dust from reaching your lungs. The tiny hairs and wet mucous in your nose will stop these things from reaching the lungs and causing infection. Stay hydrated and clean your nose twice daily with Xlear Xylitol Nasal Spray. Reduce alcohol intake and increase water intake to maintain adequate hydration. Drinking water keeps the mucous flowing and working to filter through the nose. Dehydration dries the mucous, slowing the flow and reducing effective filtration.
Blowing your nose removes the mucous that trapped the viruses, bacteria, spores, pollen and dust in the nose. Blow gently and only one nostril at a time. Blowing your nose is a good thing! It means your nose is working to effectively filter out the bad stuff. When the nose makes more mucous, it helps eliminate what has been trapped in the nasal filtration system – nasal hairs and mucous.
The nose also warms and moisturizes the air you breathe before it reaches the lungs. Another function of the nose is to smell. When the nose is congested or plugged, food doesn’t seem to have much taste. Smell is an important part of taste.
Be good to your nose. Nasal breathing protects you from viruses.